Blood sugar, also called glucose, is the main sugar in your blood. It comes from the food you eat and serves as your body’s primary energy source. Your blood provides glucose as fuel to all the cells in your body.
The body moderately regulates blood glucose levels to ensure that there is just enough of it to keep cells alive without oversaturating the bloodstream.
The status of blood sugar might change during the day. After eating, levels increase for around an hour before levelling off. They are at their lowest before breakfast. It is vital to keep the glucose level under control if you want to avoid type 2 diabetes, obesity, and other diseases.
Insulin is a hormone secreted by the pancreas, and your body requires insulin to use glucose for energy. Chronic lifestyle diseases occur when the body cannot use the glucose produced or the pancreas cannot secrete adequate amounts of insulin. Thus, the body accumulates a high concentration of glucose, also known as hyperglycaemia.
In contrast, hypoglycemia occurs when there is not enough glucose in your blood. Regular blood sugar monitoring comes in handy to manage both hyperglycaemia and hypoglycaemia. Any ups and downs on the scale are vital information for you to discuss with your healthcare team.
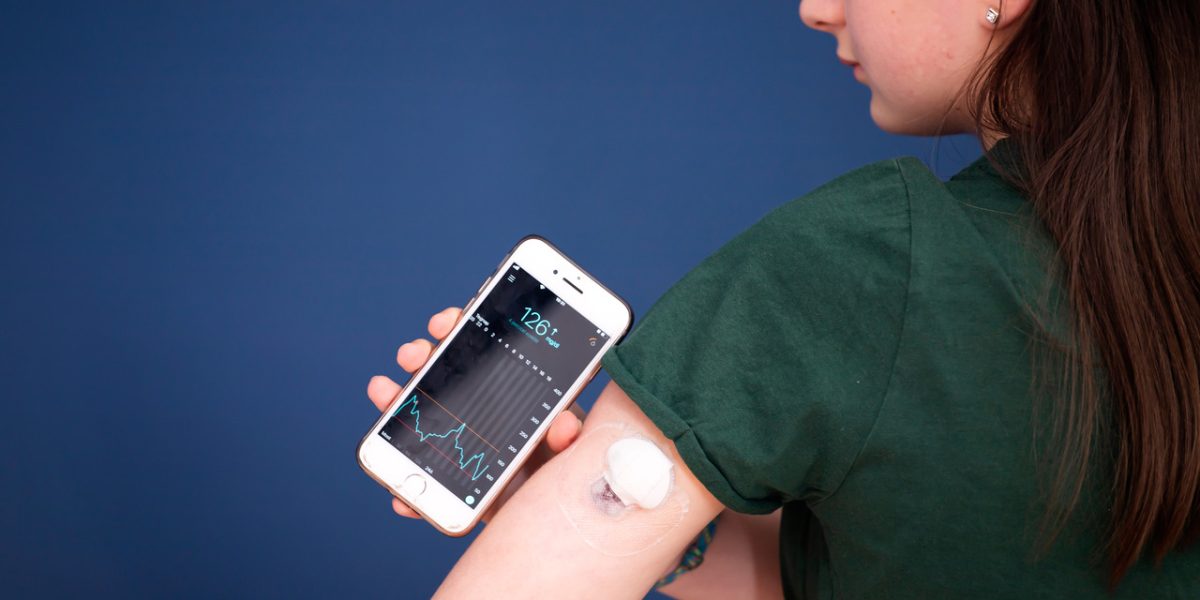
One easy glucose monitoring strategy is investing in HealthifyPro 2.0., a flagship fitness plan launched by HealthifyMe. The HealthifyPro plan includes a BIOS (a biosensor system with a Continuous Glucose Monitor) and a smart scale.
Introducing Smart Weight Loss with HealthifyPro – The Future of Fitness is Here.
✔️ Spend your calories the right way with the Pro Calorie Tracker
✔️ Know when to eat and when to burn with the Pro CGM
✔️ Understand everything about your metabolism with the Pro Metabolic Panel
✔️ Get a personalized fitness plan crafted by your Pro Coaches
✔️ Measure 11+ parameters of weight loss with the Pro Smart Scale HealthifyWithPro now!
From the tiniest nibble to the final sip of water, it can keep track of your blood sugar levels. It provides the data of glucose patterns per your food intake and other fitness activities to create a customised plan.
HealthifyMe Pro will also give you access to a nutritionist and exercise coach that you can connect with, helping you follow a personalised diet and fitness plan to reach your health goals.
Causes for Glucose Spike
You primarily digest food to turn it into glucose. Your body needs glucose because it is the fuel that keeps your muscles, organs, and brain in good working order. To be used as fuel, glucose must first enter your cells.
Insulin, a hormone secreted by the pancreas, induces cells to unlock, allowing glucose to enter. Without insulin, the glucose in your system keeps circulating, building up over time, and finding nowhere to go. Sugar accumulation in your bloodstream increases your blood glucose (blood sugar) levels.
Factors Affecting Hyperglycemia
- A lunch or snack that has an excessive amount of carbohydrates
- Lack of exercises
- Insufficient insulin or oral diabetes therapies
- Adverse effects of additional medications, like steroids or antipsychotics
- Your body generates hormones that raise blood sugar levels
- Stress, anxiety and depression
- Short-term or persistent pain
- Menstruation cycle in women
- Dehydration
Factors Affecting Hypoglycemia
- Not enough calories, such as not enough carbohydrates in a meal or snack or skipping a meal or snack
- Alcohol, when consumed on an empty stomach
- Using excessive amounts of insulin
- Adverse effects of other medications
- More physical activity than usual—physical activity improves insulin sensitivity and decreases blood sugar levels in people.
The HealthifyMe Note
Checking your blood glucose levels is essential to prevent further health issues. Some of the main reasons for its spike (hyperglycemia) are bingeing on high caloric food, alcohol, and adverse side effects of medicines, to name a few. A fall in glucose levels (hypoglycemia) occurs from skipping meals, medication side effects, and a long duration of strenuous exercise.
Ideal Blood Glucose Levels
Fasting blood sugar levels typically fall between 70 mg/dL (3.9 mmol/L) and 100 mg/dL (5.6 mmol/L). Dietary modifications and lifestyle changes are imperative when fasting glucose levels are between 100 and 125 mg/dL (5.6 to 6.9 mmol/L).
Hypoglycemia occurs when the fasting blood glucose level is below 70 mg/dL (3.9 mmol/L). Hyperglycemia occurs when the fasting glucose level is greater than or equivalent to 125 mg/dL. (going at least eight hours without eating). Children, teenagers, and expecting mothers may all have different levels.
The ideal range for most diabetic people is 80-130mg/dL in the morning before eating and between meals if more than 4 hours have passed since the last meal. It is normal for blood glucose levels to rise after eating. The goal is to keep the glucose levels under 180mg/dL 1-2 hours after the meal. The ideal blood sugar targets may get adjusted depending on individual needs or the risk of low blood sugar.
Understanding Glucose Monitoring
With the rise in poor lifestyle choices, lifestyle diseases are rapidly growing. Regularly checking glucose levels lets you know what makes it increase or decrease, such as eating different kinds of food, exercising properly, and taking prescribed medicine on time.
One can use glucose metres to do the same, and it is also possible to get A1C tests, which keep track of glucose levels over three months. Moreover, new devices allow continuous glucose monitoring, becoming an excellent alternative for monthly blood tests.
Monitoring blood glucose levels makes it easier to lower them if they are beyond what an individual needs. Everyone has a target blood sugar range, and it is essential to keep that target in mind while measuring your blood glucose levels.
Managing Blood Glucose Levels Naturally
Not only is it essential to keep blood glucose levels within the target range to avoid developing diabetes, but it is also essential to avoid long-term repercussions like heart and kidney diseases and even vision loss.
Consuming a nutritious and balanced diet consisting of plenty of fruit and vegetables, maintaining a healthy weight, and regular physical activity contributes to managing blood sugar levels.
Read more: Normal Blood Sugar Levels – Everything You Should Know
Other ways one can manage their levels are:
Health Management
- Consuming meals at regular intervals and not skipping them
- Choosing to consume foods that are lower in calories, saturated fat, trans fat, sugar, and sodium
- Tracking dietary intake as well as physical activity
- Drinking plenty of water instead of sugary alternatives
- Limiting alcoholic drinks
- Staying away from refined sugar and sweet treats
- Controlling food portions
Low blood sugar or hypoglycemia occurs when very little to no glucose is present in the blood. It can happen due to skipping meals, having alcohol, and taking unprescribed medication, leading to sweating, feeling very hungry, or shaking a lot. So it is vital to carry supplies for treating low blood sugar. If you feel any symptoms, check your blood sugar then and there, and call your doctor immediately.
High blood sugar, or hyperglycaemia, can occur due to poor levels of insulin release. It happens because of too much stress, eating more than usual or being ill.
Hyperglycaemia over a long period makes an individual extremely susceptible to developing other long-term and severe health conditions.
Regular Exercise
With regular exercise, you can maintain a healthy weight while enhancing your insulin sensitivity. Your bloodstream’s available sugar can be used by your cells more effectively if your insulin sensitivity improves.
Exercise also makes it easier for your muscles to use blood sugar for energy and muscle contraction. If you have trouble managing glucose levels, start by regularly checking your blood sugar levels before and after an exercise. With this, you can better understand how you respond to various situations and stop your glucose levels from swinging dangerously high or low.
A study shows that exercise can reduce blood glucose fluctuations and improve blood glucose control throughout the day. Furthermore, moderate-intensity aerobic exercise before breakfast can help reduce the morning rise of blood glucose in Type 2 diabetes patients.
Limit Your Carb Intake
The amount of carbs you eat greatly impacts your blood sugar levels. Your body transforms carbs into sugars, primarily glucose. After that, insulin helps your body use and store it as energy.
When you eat too many carbohydrates or have problems with insulin function, this mechanism can break down, and blood glucose levels can rise. Hence, individuals with diabetes need to measure their intake of carbohydrates and determine how much they need. It will assist in correctly planning the meals and improving blood sugar control.
Eat More Fibre
By delaying the digestion of carbohydrates and sugar absorption, fibre encourages a more gradual increase in blood sugar levels. There are two primary types of fibre: soluble fibre and insoluble fibre. Both are important.
Read more: High-Fibre Diet: Here’s What You Must Know
Although insoluble fibre does not help regulate blood sugar levels, soluble fibre can. Therefore, consuming a diet high in fibre can improve your body’s ability to regulate blood sugar and lower glucose levels. In the end, you might be able to manage diabetes better.
Monitor Your Glucose Intake
Monitoring your diabetes plays a crucial role in better managing blood sugar levels. It means this will not only help to keep track, but it can also help tweak your lifestyle accordingly. While regular tests are essential, using a Continuous Glucose Monitor (CGM) device is the best way to do it automatically.
Continuous Glucose Monitor: How Does it Work?
A continuous glucose monitor, or CGM, is one of the smart devices that automatically and continuously tracks blood glucose levels in an individual.
It works day and night, enabling one to track and see blood glucose levels anytime, anywhere. Not only can this help check glucose levels and how it changes over several hours or days, but it can also help create changes in lifestyle that are more suited to an individual’s health.
A small sensor gets inserted into the skin, usually on the stomach or the arm. It measures interstitial glucose level, the amount of glucose in the fluid between cells. It tests the glucose every few minutes. This information is sent wirelessly through a transmitter to the monitor. Recent technological advances have allowed this monitor to replace a tablet or even your smartphone!
A CGM device, therefore, is always on and measuring glucose levels. You can eat, sleep, shower or stand, and the device will store all the information.
Some models can identify an individual’s specific glucose levels and sound an alarm if they are too high or low. In contrast, others can note your lifestyle choices, like whether you have exercised, what you have eaten, etc. While this device tracks glucose levels on the go, it is vital to accompany its data with standard glucose metre tests to validate its trends and ensure it works properly.
The HealthifyMe Note
The Healthify Pro plan comprises a Continuous Glucose Monitor (CGM) that measures real-time glucose levels. The device constantly monitors your blood sugar levels even if you are eating, sleeping, exercising, or doing other activities. With the Biosensor System integrated into a Continuous Glucose Monitor, one can know exactly how the blood glucose levels uniquely react to foods and exercise routines.
Benefits of a CGM
In comparison to a standard glucose metre, a CGM is better in terms of
- Recording overnight sugar levels and sounding alarms when they are dangerously low or high
- Tracking high glucose levels in between meals
- Showing early morning trends in blood sugar
- Evaluating how your lifestyle affects you
- Needing fewer finger-prick tests
Essentially, it helps in managing blood glucose levels every day. Thus, it leads to fewer blood glucose emergencies.
CGM: Who Should Use the Device?
Those who experience constant highs and lows in blood sugar will benefit from this device, but so will those with the following issues –
- Individuals on intensive insulin therapy, also known as tight blood sugar control
- Those who experience hypoglycaemia/hyperglycaemia but are unaware of its advent or its symptoms
- Individuals with fluctuating blood sugar levels without an apparent reason
- Children prone to low blood sugar levels
- Those with an insulin pump
- Pregnant women with gestational diabetes
CGM for Blood Glucose Management
Studies have shown that real-time continuous glucose monitoring has been highly effective compared to self-monitoring of blood glucose in type 1 diabetes patients. Further, CGM has also shown to be more effective than self-monitoring in glycemic control in type 2 diabetes patients.
Further analysis also maintains the direct link of CGM devices in lowering risks of glucose level fluctuations and an actual reduction in hypoglycemia in patients with type 1 diabetes.
Research has also validated the accuracy and reliability of a CGM device, highlighting the fact that CGM can detect abnormalities in glycemic control that have not been possible before.
In addition, a study that has used a CGM device shows that it can reduce blood glucose level emergencies in critically ill patients and intensive care units. Therefore, it is reasonable to deduce that using a CGM makes a monumental difference in naturally lowering blood glucose levels and sometimes even increasing them when necessary.
Understanding the trends in an individual’s blood glucose levels makes it easier to plan how one needs to approach their lifestyle. A CGM device covers early morning spikes, nocturnal hypoglycemia trends, and of course, the daily glucose levels of an individual. Through this, it becomes easier to manage blood glucose levels.
One has all the data they need in front of them, and they need not waste their time and energy on finger tests throughout the day, week or month!
Potential Risks Associated With CGM
There are no such risks associated with using a CGM device. However, non-invasive devices such as the current technology of CGM might have sensor sensitivity and accuracy problems.
Research and technology have long evolved, and the glucose metre holds the same significance as CGM devices. CGM devices are more expensive than glucose metres and usually not present in most healthcare plans. However, due to its constant and instantaneous data, it is more cost-effective than using finger-prick tests multiple times a day.
Conclusion
A CGM device will complement your well-being journey, not dictate it. One has to know all the risks, benefits, symptoms and information before committing to one. It is possible to lower blood glucose levels naturally, and this device will provide you with data so you can independently do so.
There are many options in the market, and a particular device may fail to work for you. However, consult an expert in such cases, and decide based on all the facts.
In closing, keeping track of your blood glucose level is extremely important. If an individual goes unaware of high or low levels, it can be detrimental to their body and life. Therefore, it is essential to be aware of your health and make good choices for your well-being.